Thalassemia: A Comprehensive Guide
Introduction
The inherited blood disorder
thalassemia produces abnormal hemoglobin which results in red blood cell death
and develops into anemia. Genetic inheritance causes this disorder among
millions of individuals throughout the world particularly among people from
Mediterranean, South Asian, African, and Middle Eastern populations. Patients
with thalassemia experience different levels of disease severity which requires
treatment ranging from minimal medical needs to persistent lifelong medical
supervision.
This article examines thalassemia from
multiple angles by discussing its different forms and origin factors as well as
its diagnostic signs and treatment plans together with prevention strategies.
Types of
Thalassemia
The classification of Thalassemia
depends on which area of the hemoglobin molecule becomes mutated. The protein
structure of hemoglobin includes two primary elements known as alpha-globin
together with beta-globin. Thalassemia exists in two main types according to
the defective chain between alpha-globin and beta-globin.
1.
Alpha-Thalassemia
Alpha-thalassemia develops when people
lack either some or all of their alpha-globin chain proteins. The number of
mutated alpha-globin genes determines the level of severity in patients.
·
The presence of
one defective gene in Silent Carrier status results in no visible signs and
makes them carriers of the condition.
·
People with
Alpha-Thalassemia Trait who have two genes affected will experience mild anemia
that medical professionals might mistake for iron deficiency.
·
Thalassemia
patients with three affected genes are diagnosed with Hemoglobin H Disease
which leads to moderate to severe anemia that causes fatigue and causes their
spleen to enlarge.
·
The condition of
Hydrops Fetalis leads to death before or shortly after birth because of severe
anemia in individuals with four affected genes.
2.
Beta-Thalassemia
The beta-thalassemia disease appears
when mutations affect the beta-globin genes. The extent of the condition
depends on the number of affected beta-globin genes.
·
Individuals
having Beta-Thalassemia Minor with one affected gene show minimal anemia while
remaining carriers of the condition.
·
Beta-Thalassemia
Intermedia affects two partially mutated genes leading to moderate anemia that
sometimes needs occasional blood transfusions.
·
Patients having
Beta-Thalassemia Major (Cooley’s Anemia) (2 genes severely affected) face a
life-threatening condition that needs ongoing blood transfusions with medical
supervision.
Causes and
Genetics
A child requires inheritance of
defective genes from both parents to develop severe thalassemia since this
condition appears as an autosomal recessive disorder.
·
The risk that
both parents being carriers (thalassemia minor) creates the following
possibility:
·
Thirty percent of
their offspring will develop thalassemia major according to the genetic
information.
·
Their offspring
has a 50% possibility to become a carrier.
·
A 25% risk exists
for their offspring to remain unaffected from the disorder.
The HBB gene (beta-thalassemia) and
HBA1/HBA2 genes (alpha-thalassemia) mutations cause problems with hemoglobin
production that creates dysfunctional red blood cells which the body destroys
too early.
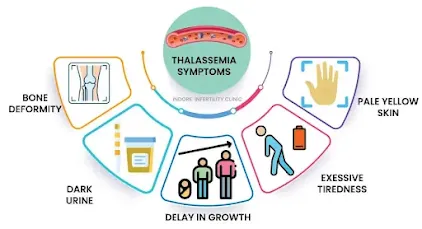
Symptoms of
Thalassemia
The types and severity of thalassemia
determine which symptoms will appear in patients.
Mild Thalassemia
(Minor/Trait)
·
Mild anemia
·
Fatigue
·
Pale or yellowish
skin (mild jaundice)
Moderate to
Severe Thalassemia (Intermedia/Major)
·
Severe anemia
·
Growth delays in
children
·
Bone deformities
(especially in the face and skull)
·
Enlarged spleen
and liver
·
Dark urine (due
to excessive red blood cell breakdown)
·
Frequent
infections
·
Heart problems
(due to iron overload from transfusions)
Diagnosis
Proper management of thalassemia
requires prompt detection of the condition. Diagnostic methods include:
1. Blood Tests
·
Complete Blood
Count (CBC): Detects low hemoglobin and abnormal red blood cell size.
·
Hemoglobin
Electrophoresis: Identifies abnormal hemoglobin variants.
·
The testing of
reticulocyte Count provides information about bone marrow activity through the
measurement of young red blood cells.
2. Genetic
Testing
·
Tests validate
alpha or beta-globin gene mutations.
·
Helps in prenatal
screening for at-risk couples.
3. Prenatal
Testing
·
Healthcare
providers conduct Chorionic Villus Sampling (CVS) between weeks 11 and 14 of
pregnancy.
·
The procedure of
Amniocentesis occurs during weeks 15 to 20 for examining fetal DNA.
Treatment Options
The medical approach to thalassemia
treatment depends on its classification type and its severity level.
1. Blood
Transfusions
·
Individuals who
have thalassemia major along with some intermediate cases need this treatment.
·
The treatment of
thalassemia requires regular blood transfusions to prevent the development of
low hemoglobin levels.
2. Iron Chelation
Therapy
·
Organ damage
occurs because of the excessive transfusions that cause iron overload in the
body.
·
Chelating agents
(Deferoxamine, Deferasirox, Deferiprone) remove excess iron.
3. Bone Marrow or
Stem Cell Transplant
·
The only
potential cure for severe thalassemia.
·
Treatment
requires finding a suitable donor who usually needs to be a sibling.
4. Gene Therapy
(Experimental)
·
The use of CRISPR
and viral vector technologies continues to develop as new approaches for fixing
defective genes.
5. Supportive
Treatments
·
People who take
folic acid supplements receive help for red blood cell production.
·
The surgeon
removes the spleen when it becomes excessively active.
·
Hormone Therapy:
For delayed puberty due to thalassemia.
Complications of
Thalassemia
The absence of appropriate treatment
allows thalassemia to produce the following issues:
·
The accumulation
of iron causes serious damage to the heart together with the liver and
endocrine system.
·
Bone Marrow
Expansion Causes Deformations of the Bones.
·
Heart Disease:
From anemia and iron buildup.
·
The removal of
the spleen increases infection risks specifically.
·
Delayed Growth
& Puberty: Due to chronic anemia.
Prevention and
Genetic Counseling
The prevention of thalassemia requires
genetic carrier detection together with proper family planning strategies.
·
Pre-Marital
Screening: Identifies carriers before marriage.
·
Prenatal Testing:
Detects thalassemia in the fetus early.
·
PGD serves as a
technique with IVF that selects healthy embryos.
Living with
Thalassemia
Thalassemia patients can achieve life
fulfillment when they receive proper medical attention.
·
Medical
professionals should perform periodic examinations to track iron levels
together with organ system functioning.
·
A balanced diet
rich in calcium, vitamin D, and antioxidants.
·
Patients should
restrict their consumption of iron-rich foods during transfusion treatment.
·
Patients need
psychological assistance to deal with their ongoing health condition.
Conclusion
The genetic disorder called
thalassemia represents a serious condition which patients can effectively
manage. Better results for thalassemia patients now seem possible because
medical research continues to make progress through gene therapy and enhanced
chelation treatment methods. Individuals with thalassemia can enhance their
quality of life through early recognition of the condition and proper genetic
advice and strict adherence to recommended medical regimens.
The implementation of screening
programs together with awareness campaigns will decrease the weight of
thalassemia while ensuring better health outcomes for upcoming generations.
References
·
National Heart,
Lung, and Blood Institute (NHLBI)
·
World Health
Organization (WHO)
·
Thalassemia
International Federation





Post a Comment
0Comments