Measles: A Comprehensive Overview of Causes,
Symptoms, Complications, and Prevention
Introduction
Measles is a highly spreadable disease
called rubeola that is mostly seen in kids, but unvaccinated individuals of all
ages can get it too. Even though a vaccine exists, measles is still a big
health concern in areas where not many people get vaccinated. The virus that
causes measles is part of the Paramyxoviridae family and is spread when people
breathe in infected droplets.
Here, we look closely at measles,
discussing its origins, spread, symptoms, complications, methods of diagnosing
it, treatment options and ways to stop it from spreading.
1. Etiology and
Transmission
1.1 The Measles
Virus
The measles virus is an RNA virus from
the genus Morbillivirus. It spreads very easily, since R₀ is estimated at 12-18
which means each one infected might spread it to 12 to 18 people who have not
had the virus yet.
1.2 Modes of
Transmission
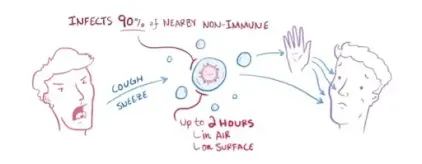
Measles is spread by:
·
Droplets that are
airborne when someone coughs or sneezes
·
Infection can
happen when nose or throat secretions from an infected person touch your mouth
or nose.
·
If you touch
anything infected, the virus may still be active for up to two hours.
Someone who has chickenpox can infect
others from four days before they show the rash for up to four days afterward.
2. Clinical
Presentation and Stages of Measles
Each part of the illness called
measles is marked by its own set of symptoms.
2.1 Incubation
Period (10-14 days)
After a person is infected, the virus
takes 10-14 days to develop symptoms. The virus starts to multiply in your
lungs and then infects nearby lymphoid tissues.
2.2 Prodromal
Phase (2-4 days before rash)
At first, the symptoms look like those
of a major cold.
·
Fever that is as
high as 104°F (40°C)
·
Cough
·
A runny nose
(coryza)
·
Conjunctivitis is
when the eyes become red and watery.
·
Koplik’s spots
(small, white spots with blue centers on the inner cheeks) are a sure sign of
measles.
2.3 Rash Phase
(3-5 days after initial symptoms)
A maculopapular rash is first noticed
on the face (hairline and behind the ears) and then spreads to the trunk, arms
and legs. The skin lesions are flat and red and they can join as they become
larger. During this time, the person usually has their highest fever.
2.4 Recovery
Phase (7-10 days after rash onset)
Symptoms get better gradually and the
rash disappears the same way it appeared, often leaving behind a little brown
discoloration and slight peeling.
Read also: Global Polio Eradication Initiative (GPEI)
3. Complications
of Measles
Most people get better from measles,
but it can cause serious health problems in:
·
Youngsters under
the age of 5
·
People who are 20
years old or older
·
Pregnant women
·
Immunocompromised
individuals
·
Patients with a
lack of vitamin A
3.1 Common
Complications
·
Diarrhea and
vomiting (that can cause dehydration)
·
Otitis media is
an ear infection that sometimes results in hearing loss.
·
Laryngotracheobronchitis
(croup).
·
Measles
infections are most likely to result in death because of pneumonia.
3.2 Severe and
Life-Threatening Complications
·
One percent of
encephalitis cases (1 in 1,000) end in death (15%).
·
Subacute
sclerosing panencephalitis (SSPE) – a rare disease of the brain that develops
7-10 years following an infection.
·
In people with
weakened immune systems, giant cell pneumonia can cause serious trouble
breathing.
·
When pregnant
women have miscarriages or preterm births
4. Diagnosis of
Measles
4.1 Clinical
Diagnosis
A healthcare worker may use the
following to diagnose measles:
·
Fever, rash,
cough, coryza and conjunctivitis are typical symptoms.
·
If the fever is
present then Kolpik’s spots may also be present.
·
Whether the
person had contact with a measles patient recently or traveled recently to
places where the disease is common.
4.2 Laboratory
Confirmation
·
This test (IgM
antibody test) checks for a specific form of antibody related to measles.
·
RT-PCR tests for
viral RNA in samples from the throat/nose, urine or blood.
·
Because viral
culture grows slowly, it is less frequent.
5. Treatment and
Management
There are currently no medications
that treat measles infection. Managing this disease is about caring for the
patient and stopping complications.
5.1 Supportive
Measures
·
Fluids through
either oral rehydration or IV (if that’s required)
·
You should give
your child acetaminophen or ibuprofen to bring down the fever.
·
Taking vitamin, A
(helps fight severe disease and reduces deaths, mainly in people with little
vitamin A)
o
Dosage:
§ Infants under 6 months should receive 50,000
IU.
§ Children aged 6 to 11 months should get
100,000 IU.
§ Your child or adult should take 200,000 IU of
vitamin D a day.
5.2 Antibiotics
(if secondary bacterial infection occurs)
·
Amoxicillin is
often given for pneumonia or otitis media infections.
5.3
Hospitalization (for severe cases)
·
Must be used for
patients with encephalitis, severe dehydration or respiratory distress.
6. Prevention:
Vaccination and Public Health Measures
6.1 Measles
Vaccine (MMR or MMRV)
Taking two doses of the MMR vaccine is
97% likely to protect children from infection. Some countries give the MMRV
shot for measles, mumps, rubella and varicella.
·
The first time
you give the vaccine is when your child is 12 to 15 months old.
·
After the first
dose, the second one should be given 4-6 years later (or at least 28 days after
the first).
6.2 Post-Exposure
Prophylaxis
·
Getting
vaccinated within 72 hours after exposure can help avoid or lessen the chance
of disease.
·
For high-risk
peoples (infants, pregnant women, immunocompromised patients), IG should be
given within 6 days.
6.3 Herd Immunity
and Global Eradication Efforts
·
Herd immunity
threshold requires about 95% of the population to get vaccinated.
·
The WHO is
striving for global measles elimination, but outbreaks keep happening for
several reasons.
o
Vaccine hesitancy
o
Healthcare
systems that lack strength
o
Areas where
vaccination is disrupted
7. Measles
Outbreaks and Current Epidemiology
Even after being declared gone in the
U.S. in 2000, outbreaks of malaria are still possible.
·
Cases brought
into the country from abroad
·
People who do not
get vaccinated such as religious or anti-vaccine groups
7.1 Recent
Outbreaks
·
In 2019, there
were 869,000 cases globally which was the most since 1996.
·
This year in the
U.S., there have been clusters of unvaccinated children infected in Ohio,
Minnesota and New York.
7.2 Global Burden
·
Before
vaccination was available, measles killed an average of 2.6 million people per
year.
·
During 2022, most
malaria deaths took place in low-income countries, adding up to about 136,000
deaths.
8. Myths and
Misconceptions About Measles
8.1 Measles is
just a mild childhood illness.
·
Reality: This
condition can end in complications that may be dangerous or even deadly.
8.2 The MMR
vaccine causes autism.
·
In reality, lots
of big studies (including CDC and WHO) have shown that the myth about MMR and
autism started with a fraudulent 1998 study by Andrew Wakefield.
8.3 Natural
infection is better than vaccination.
·
Reality: Getting
sick from measles is dangerous, but vaccination keeps you safe.
9. Conclusion
Vaccination can prevent people from
getting measles which is still a dangerous disease. Of all solutions,
vaccination is the best way to stop the spread, reduce symptoms and save lives.
The main goal of public health should be:
·
Reaching more
people around the world with vaccines
·
Combating
misinformation
·
Increasing the
ability of countries to deal with outbreaks
If countries remain alert and
vaccinate most people, measles could be eliminated everywhere, saving many
lives.
References
·
The World
Health Organization (WHO) has Measles Fact Sheets.
·
CDC Measles
Guidelines
·
Lancet –
Research on Measles Epidemiology
·
Journal of
Infectious Diseases – Measles and How to Treat Its Complications







Post a Comment
0Comments